A Comprehensive Guide to Cognitive Behavioral Therapy (CBT)
Summary
Cognitive Behavioral Therapy (CBT) is a structured, goal-oriented treatment targeting depressive thoughts and behaviors. Initially developed in the 1960s to treat depression, its use has expanded to anxiety, addiction, and OCD. Technology, like virtual reality and AI chatbots, is being integrated into CBT, but human therapists remain crucial for personalized care and real-time adjustments.
Key insights:
Introduction to CBT: CBT is an evidence-based treatment aiming to change unfavorable thought and behavior patterns. CBT, which was derived from cognitive and behavioral therapies in the 1960s, is useful for treating psychological and post-trauma disorders and has advanced with technology to include apps and online platforms that increase accessibility.
Core Principles and Theoretical Foundation: The foundation of Cognitive Behavioral Therapy (CBT) is the idea that our perceptions of events, not the events themselves, determine our emotional reactions and behaviors. It focuses on recognizing and altering maladaptive beliefs and actions using methodical, goal-oriented techniques to reduce emotional distress and enhance mental health.
Conducting CBT: The first step in the CBT process is an assessment to identify the patient's problems and establish realistic goals. During sessions, issues are discussed, cognitive distortions are noted, and feedback is given. Assignments for homework are essential because they enable patients to use newly acquired skills in practical settings.
CBT Techniques and Methods: Behavioral activation to promote positive behaviors, cognitive restructuring to counter negative thoughts, and mindfulness exercises to reduce stress are important components of cognitive behavioral therapy. Tracking and evaluating thoughts and behaviors for successful intervention is made easier with the use of journals and thought logs.
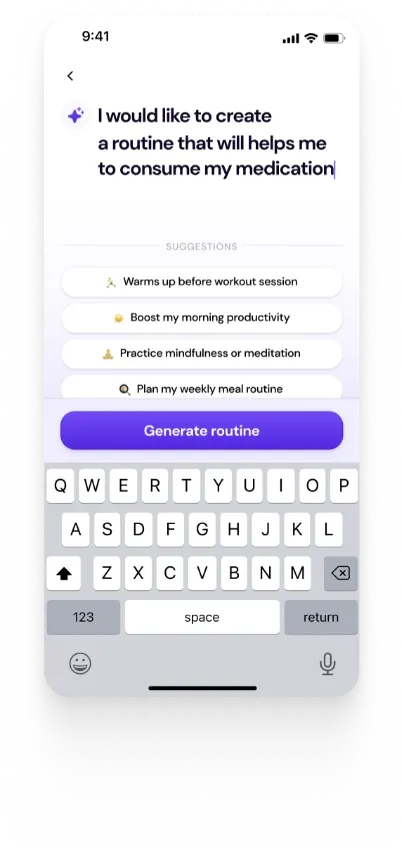
Digital Age and CBT: CBT is becoming more widely used as a result of access to online resources like BetterHelp, Talkspace, and Woebot. Though questions concerning efficacy and data privacy persist, these tools combine technology and human support to offer flexible, on-demand mental health care through automated and virtual therapy options.
Human Involvement vs. Technology: Although technology can automate repetitive CBT tasks and offer round-the-clock support, it cannot take the place of human therapists' subtle, compassionate care. In order to manage complex emotional responses, customize therapy, and make in-the-moment adjustments based on patient needs, human involvement is essential.
Introduction
An inclusive approach to address a broad spectrum of psychological challenges remains immensely instrumental. The therapeutic approach to mitigate psychological disorder has been on the rise across the world mainly due to the multi-dimensional nature of its interventional approach and surging cases of psychological stress amongst the populace.
Cognitive Behavioral Therapy (CBT) is considered a significant milestone in the advancement of psychological treatment, embodying pivotal ideals of psychotherapy and following an evidence-based approach to support people in addressing negative thought patterns and behaviors. Likewise, it follows a methodical and goal-oriented approach, with the intention of lowering symptoms by altering people's perspectives and responses to difficult circumstances.
The 1960s saw the emergence of CBT, which combined ideas from behavioral and cognitive therapies. It was first created to treat depression but is now extensively used to treat a variety of other mental health issues. Likewise, CBT is still a mainstay of modern mental health care and its efficacy in alleviating symptoms has made it the go-to treatment for numerous psychological disorders. The flexibility of CBT—including "technology-empowered CBT" (tCBT), which helps get over obstacles like stigma, unavailability of therapists, and geographic restrictions—makes it even more significant. Technological integration in the CBT embodies capacity and to a large extent bolstered improvement in affordability and accessibility.
This article aims to profoundly analyze CBT as an imperative psychotherapy embodying multi-dimensional benefits, and explore the holistic impact of technology in its wide spread and efficacy.
Understanding CBT - Key Principles
1. The Theoretical Foundation Behind CBT
The therapy combines a structured, evidence-based, conversational, and motivational approach to profoundly scrutinize and develop a nexus between thoughts, feelings, ideas, and actions. Cognitive Behavioral Therapy, while being an approved therapeutic procedure, embodies significant diagnostic provisions, thus further strengthening and validating the diagnosis of a psychological disorder. Likewise, its fundamental tenet focuses on the imperative notion that emotional response to a situation is shaped by an individual's perception of the event and not by the overall details of the event.
2. Definition and Core Principles
Cognitive Behavioral Therapy (CBT) is a type of psychotherapy that focuses on the interconnection of cognitive patterns, feelings, behaviors, and thoughts that drag an individual into a vicious negative cycle of anxiety. CBT offers resolution to the stress disorder by capacitating an individual to systematically deal with overwhelming problems in a unique way that allows further breaking down of problems into smaller parts. Likewise, CBT is based on Beck's (1964) Cognitive Model, which postulates that faulty thought processes are the cause of mental suffering. It further distinguishes between three levels of cognition that include: a) Negative Automatic Thoughts (NATs), b) Dysfunctional Assumptions, and c) Fundamental Beliefs. These presumptions and beliefs, formed and shaped by prior experiences, affect people's perceptions of and responses to circumstances, resulting in emotions and behaviors that are maladaptive.
3. How CBT aims to change thinking patterns
The foremost objective of Cognitive Behavioral Therapy is to help individuals recognize and resist negative thought patterns, like those associated with anxiety or depression. This resistance is further linked to using the strength of the mind and inner self to unlearn the specific troublesome thoughts that exacerbate the thought process. Moreover, by opposing these notions and embracing more reasonable and alternative viewpoints, people can put an end to their emotional suffering. As a result of CBT, patients get to explore and develop a concrete understanding of the relationships between their thoughts, feelings, and behaviors.
This process helps them to manage the symptoms of mental health conditions by addressing the root cause of their emotional responses that come from an over-sensitive use of the mind and problematic thoughts. CBT makes use of behavior strategies like behavioral experiments, graded tasks, and activity scheduling. People can test their catastrophic predictions, get back into daily activities, and gradually alter their thoughts and behavior with the help of these interventions.
Conducting Cognitive Behavioral Therapy (CBT)
1. Initial Assessment - Analyzing Issues and Goals
The goal of the first phase of Cognitive Behavioral Therapy (CBT) is to identify the patient's problems and lay the groundwork for treatment by establishing specific objectives. During this phase, the therapist conducts a thorough psychological state assessment, focusing on the patient's existing condition, nature of thoughts, ongoing behaviors, and gravity of emotional reactions.
The primary aim of this evaluation is to pinpoint the specific uncontrolled pejorative thoughts, cognitive distortions, and problematic core beliefs that contribute to the patient's distress. In order to attain this, the therapist may ask in-depth analytical questions about the patient's past experiences, ongoing issues, and further talk about the therapy goals.

Based on the assessment, the patient and therapist collaboratively establish SMART (specific, measurable, achievable, relevant, and time-bound) goals for therapy. The therapist and the patient agree on the established diagnosis and the actionable treatment plan, which is flexible and amendable based on emerging situations and challenges.
2. Dedicated Structured Sessions
CBT is extremely regimented, with each session adhering to a predetermined structure, thus ensuring that the therapy remains targeted and effective. A typical CBT session structure is composed of a quick initial assessment of the patient's state of mind, any changes from the previous session, and a review of homework done at the start of each session. Together, the patient and therapist create a session schedule that gives priority to the most important concerns.
Throughout, the therapist offers summaries to help patients understand important points and make sure they are actively participating in the process. CBT sessions are usually scheduled once a week and last approximately sixty minutes. The majority of treatment plans call for 8 to 12 weeks of therapy, however, this can change depending on the patient's progress and the severity of their problems. Depending on the needs of the individual, sessions may be modified or prolonged.
3. Homework and Exercises relevant to CBT
A crucial part of Cognitive Behavioral Therapy (CBT) is an initial homework, which serves to both reinforce the skills acquired in therapy and assist the patient in applying them to everyday situations. CBT poses a strong value in the practice outside of the therapy room. Patients can use behavioral and cognitive strategies in their daily lives through homework, which makes them more conscious of their thoughts and actions. This is essential for bringing about long-lasting change because it reinforces the skills acquired in therapy.
Assignments usually consist of thought journals, in which patients document and examine their automatic ideas and cognitive distortions, behavioral experiments, which assess the precision of negative forecasts, and exposure tasks, which involve gradually facing anxiety-inducing circumstances under supervision. Additional workouts could include structured activities designed to promote the adoption of positive behaviors or mindfulness techniques.
Methods and Techniques in CBT
1. Cognitive Restructuring or Reframing
Cognitive restructuring entails identifying negative thought patterns that result in emotional distress and counterproductive behaviors. Together with the patient, the therapist seeks to identify cognitive distortions like extreme thinking, overgeneralization, and catastrophizing.
After the patient recognizes these thoughts, the therapist works with him/her to refute and reframe the ideas in a way that is more realistic and constructive. In this approach, the patients are counseled, taught, and reinforced to replace negative thoughts such as "I always fail" with more realistic ones like "Sometimes I succeed, and I can learn from my mistakes", through this process.

2. Exposure Therapy
In a safe setting, exposure therapy is used to capacitate patients in facing their anxieties and fears. Pursuing small steps at a time, the therapist exposes the patient to the feared object, circumstance, or memory that generates negative thoughts and energy. The patients benefit from less avoidance behavior and desensitization as a result. A person who is afraid of public speaking, for instance, might begin by visualizing speaking in front of others, work on it in front of a mirror, and then give a speech to a small group of people. As a result of repeated exposure, the person becomes more confident in their capacity to handle the fear and the anxiety that goes along with it.
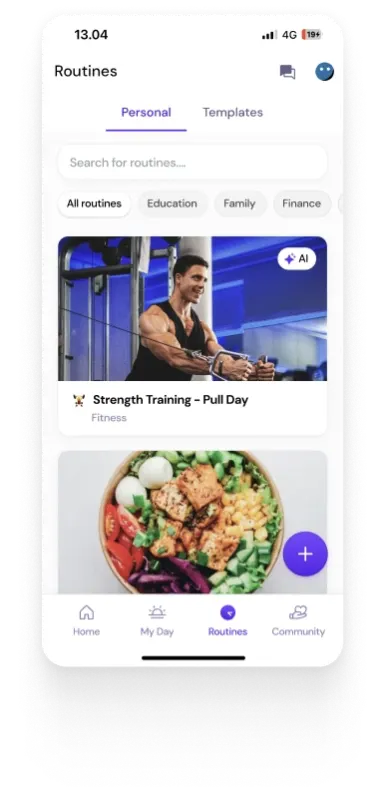
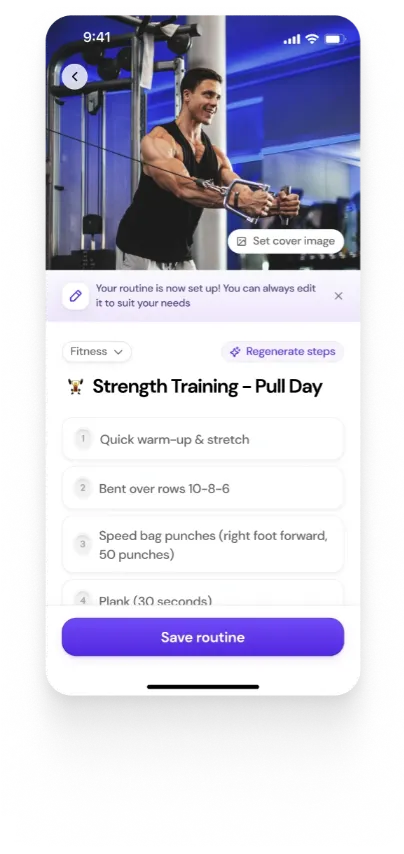
3. Behavioral Activation
Behavioral activation places a strong emphasis on partaking in activities that are likely to elevate mood and lessen symptoms of depression. These activities, which can include hobbies, physical activity, and social interactions, are scheduled and gradually the incidence is increased with the participation of the patient in collaboration with the therapist. Therefore, the resumption of constructive activities helps patients feel better and fosters higher motivation and involvement.
4. Mindfulness and Relaxation Techniques
Mindfulness practices are frequently employed in CBT to assist patients in becoming more cognizant of their thoughts and emotions without getting affected. This particular modality is immensely beneficial for stress, anxiety, and depression management. To ease physical stress and encourage calmness, relaxation techniques like progressive muscle relaxation, deep breathing, and visualization are also included. These methods work well for handling stress in general as well as phobias and social anxiety.
5. Problem-Solving Therapy
The patients undergoing problem-solving therapy interact with everyday obstacles that lead to tension and anxiety. In this modality, patients are trained to recognize possible solutions, dissect issues into smaller and more manageable components, and methodically assess the best course of action. This method works especially well for people who feel overpowered by daily obstacles and provides them with more self-assurance in their capacity to overcome obstacles.
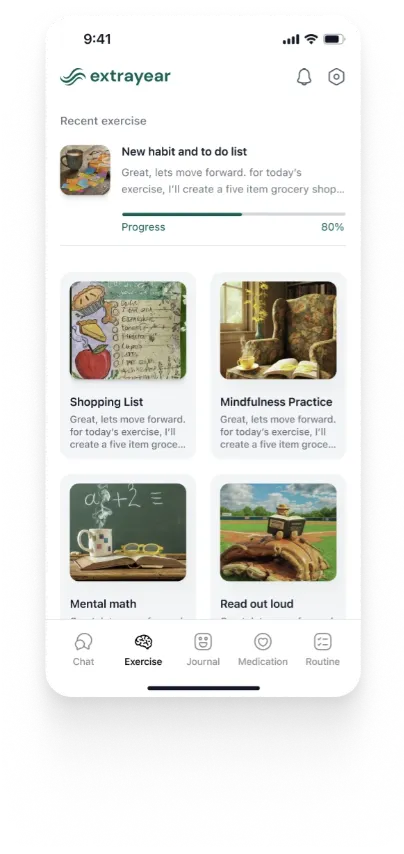
6. Journaling and Thought Records
One important CBT technique is Journaling, which encourages patients to keep a weekly log of their varying thoughts, feelings, and behaviors. Keeping a thought journal enables people to monitor their automatic negative thoughts, the circumstances that set them off, and the feelings that ensue. Patients and therapists can work on rephrasing negative thoughts and spot patterns by going over these records. Likewise, a patient can try to challenge a belief like "I'm not good enough" before social interactions by thinking something more balanced, like "I may not be perfect, but I have qualities that others appreciate."
CBT in the Digital Age
1. Electronic Resources
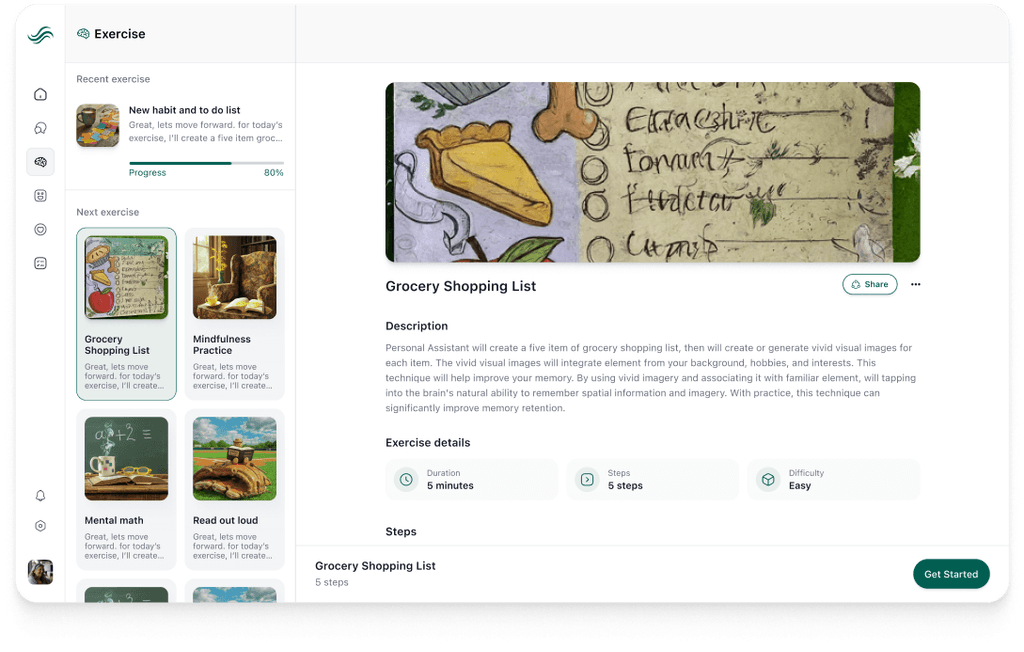
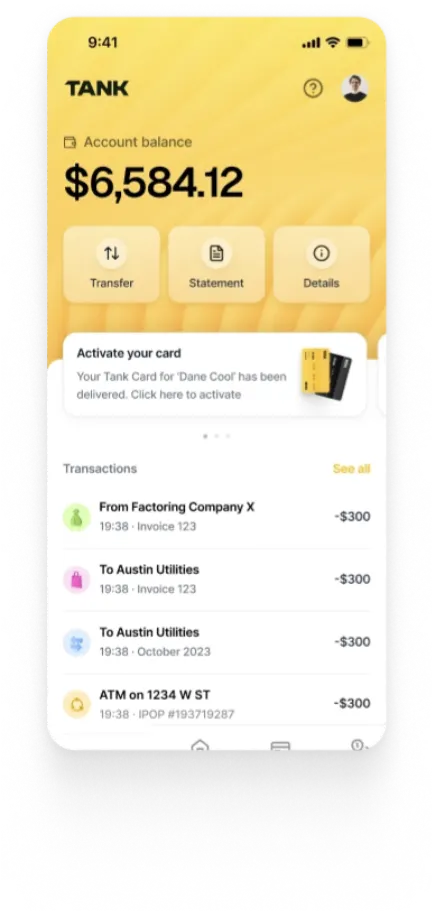
Electronic resources for cognitive and psychotherapy have expanded access to mental health care through the development of digital products and in this regard have developed dedicated technological platforms for Cognitive Behavioral Therapy (CBT). Platforms like Talkspace, BetterHelp, and Woebot are prime examples of how technology is being used to operationalize and apply CBT methods.
Woebot, an AI-powered chatbot, offers psychoeducation and guides users through structured exercises to teach CBT techniques. It is designed to simulate conversational therapy by providing coping mechanisms for stress, anxiety, and depression in real time through effective text-based interactions. Woebot is free to use.
BetterHelp and Talkspace, on the other hand, facilitate virtual therapy sessions by connecting users with certified therapists. These platforms combine traditional therapy with CBT techniques, allowing clients to access professional therapeutic support while remaining home. This approach helps overcome logistical challenges such as travel, time, or stigma by enabling clients to engage in therapy without visiting a facility in person. These platforms often provide psychoeducation and CBT techniques through worksheets, personalized exercises, and real-time interaction, offering hybrid care that combines human support and technology to give patients more options for receiving therapy.
BetterHelp operates through different channels including:
Messaging. Allows the user to send your counselor a private message at any time using the messaging function in your therapy room. This message isn’t live chat, so the therapist may not respond immediately.
Phone sessions: It allows the user to schedule a phone session using the calendar function in the therapy room, which displays your therapist’s availability.
Video sessions: with phone and live chat sessions, the user must schedule a video session using the calendar function in the therapy room.
Live chat. The user can also schedule a live chat session with the counselor via the calendar function.
Talkspace, on the other hand, offers services personalized to individuals, couples, LGBTQIA+, veterans, and teen therapy. Communication occurs through online video calls or messaging sessions with the therapist. Talkspace is also connected to many major insurance providers, which can increase affordability for insurance-protected categories.
Both Talkspace and BetterHelp allow customers to change therapists at any time and as many times as they find necessary.
BetterHelp is priced at $65 to $90 per week, while TalkSpace ranges from $69 to $109. Unfortunately, although these options are still cheaper than traditional counseling sessions, many families may not be able to afford them. Hence, households with lower incomes are the most penalized by this, which defeats the purpose of providing higher levels of accessibility through online support.
2. How Digital Platforms Deliver CBT Techniques
The application of AI and virtual reality (VR) in cognitive behavioral therapy (CBT) is rapidly developing. Artificial Intelligence and Chatbots: AI uses structured dialogues and automated responses, as demonstrated by Woebot, to lead users through CBT techniques. These systems interact with users through Natural Language Processing (NLP), providing interventions in times of distress akin to those provided by a human therapist.
The platforms aim to help users adopt coping mechanisms, confront cognitive distortions, and instantly control their emotions. Even though AI cannot empathize as deeply as a human therapist, it still offers a scalable and easily accessible alternative for prompt mental health assistance.
VR is being used more and more in CBT for exposure therapy, particularly for PTSD and phobias. It allows patients to face anxieties or upsetting memories in a safe, virtual setting. Through the simulation of real-world exposure to feared stimuli in a more controlled and safe environment, this immersion aids in the reduction of anxiety. When compared to conventional in-office methods, VR exposure can be customized to meet specific needs and provide an engaging therapeutic experience that could expedite the course of treatment.
3. Pros and Cons of Digital CBT
The capacity of digital cognitive behavioral therapy to bridge the accessibility gap in mental health treatments is one of its greatest advantages. Platforms have the capacity to reach a global audience, removing the barrier of distance from therapy sessions for those living in underprivileged or distant places. Furthermore, because these services (such as 24/7 chatbot access and on-demand therapy) are instantaneous, users can engage with CBT as soon as symptoms emerge, eliminating the waiting periods that come with traditional therapy.
Since so many people use cell phones, therapy can be given whenever and wherever symptoms appear. This removes barriers like having to take care of children, traveling, and missing work. Moreover, app-based solutions can reduce the stigma associated with attending therapy sessions since users can communicate privately with mental health providers.
Digital CBT is not without its drawbacks, either. Engagement is a big problem because many people download an app but do not use it often. For example, just 15.6% of users of the PTSD Coach app engaged with it one week after downloading it. Furthermore, some digital products do not have enough clinical supervision or empirical backing. Although I-CBT and related methods have demonstrated efficacy, the lack of a live therapist may diminish the customized attention and flexibility that conventional in-person therapy offers.
The paucity of solid data supporting many digital technologies for mental health is another issue. For example, efficacy evidence for the majority of mental health apps now on the market is scarce. Furthermore, concerns about privacy and data security are getting more and more important because a lot of apps gather private health data without explicit user authorization or data protection regulations.

Human Involvement vs. Technology in CBT
We will now discuss the relationship between human involvement and technology in CBT and how the two can complement each other, starting with the role of technology:
Automating Routine CBT Tasks: Technology may automate several common duties in Cognitive Behavioral Therapy (CBT), including mood tracking, journaling, and even providing guided interventions. These are repetitive processes that ideally require technology solutions.
Through the use of apps such as Mood247 or T2 Mood Tracker, people can record their emotional states for subsequent evaluation by therapists, which reduces review time and improves self-monitoring accuracy. Additionally, by tracking their development over time, users of these tools might see minor but meaningful gains in their mental health thanks to the clear visualizations they provide.
Providing 24/7 Support: One of the main benefits of technology in CBT is its potential to provide 24/7 support, something that traditional treatment is unable to deliver. After traditional treatment hours, mobile apps and online resources offer prompt interventions and coping strategies. For instance, people who are depressed or anxious can use dedicated apps designed specifically for this reason to access guided breathing exercises, meditations, or grounding techniques whenever they feel distressed.
Although technology has numerous benefits in this regard, still it is not a substitute for a human therapist when it comes to treating complicated and frequently erratic emotional reactions. The management of challenging emotions including trauma or loss is a part of emotional complexity, and it imperatively requires a skilled therapist's compassionate understanding and expert advice. While technology can help by measuring moods and sending reminders, it cannot interpret emotions in a context specific to an individual. Human therapists are able to identify the complex interactions between emotions and modify their style in real time to provide consolation, affirmation, and direction.
In a more philosophical context, technology is unable to adequately replace empathy, which is essential to the therapeutic process. The in-depth conversations create an enabling environment for clients to conveniently explore their feelings by making them feel fulfilled and encouraged. Although self-guided therapies can be facilitated through mobile applications, still they cannot replicate the individualized feedback and emotional depth that a therapist can deliver. Moreover, therapists play an immensely crucial role in assisting clients in making sense of their experiences by prudently and perceptively leading them through therapeutic exercises.
As the treatment advances, the demands and the underlying obstacles change, thus necessitating quick and flexible modifications to treatment plans. In this regard, a mobile application might offer fixed interventions according to pre-established standards, but a human therapist can dynamically modify the therapeutic process in response to patient input as well as advancement, or regression. For example, a therapist can immediately alter a treatment plan if a patient exhibits indicators of declining mental health, something that an app cannot do. The capacity to adjust in real time guarantees that therapy will continue to be responsive and successful for each patient's individual path.
In summary, technology has an impactful role in providing online psychotherapy support and has been instrumental in automating certain chores and providing ongoing assistance, but human interaction is still essential for delivering the individualized, compassionate, and flexible care required for successful therapeutic outcomes. The most effective strategy blends the advantages of both, with technology supporting rather than taking the place of the therapist's job.
Outcomes and Effectiveness of CBT
The effectiveness of Cognitive Behavioral Therapy (CBT) has been well-established and scrutinized extensively in relation to a wide range of mental health issues. In general, CBT is quite beneficial for treating stress, bulimia, anxiety disorders, somatoform disorders, and problems controlling aggression. It performs better than other therapies in terms of response rates, and reports of major gains in functioning and symptom reduction are common.
However, depending on the particular issue, CBT's efficacy varies. CBT is less effective than other treatments for certain diseases, including bipolar disorder and schizophrenia. Furthermore, even though CBT has demonstrated promising results in numerous domains, additional high-caliber research and CBT strategy optimization for specific issues remain necessary.
1. CBT for PTSD
Research has shown that Cognitive Behavioral therapy (CBT) is a successful treatment for Post-Traumatic Stress Disorder (PTSD). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses shows that CBT has a significant positive impact on PTSD symptoms, especially when paired with exposure therapies. The response rates of CBT varied between 38% for treating obsessive compulsive disorder and 82% for treating body dysmorphic disorder. Research demonstrates that CBT and EMDR (eye movement desensitization and reprocessing) are equally effective in treating PTSD, with both techniques surpassing conventional interventions such as supportive counseling.
The paper presents a comprehensive outcome table comparing the response rates of Cognitive Behavioral Therapy (CBT) to various other treatment options. These include medication (MED), other therapies (OT), placebo/control treatments (PBO), treatment as usual (TAU), and waitlist treatment (WT). The results, expressed as percentages, demonstrate the relative effectiveness of CBT against these alternative approaches.
CBT has a typically high success rate in treating PTSD, with notable improvements shown in symptoms and general functioning. Long-term results seem to be positive as well, while some research indicates that CBT may lose its effectiveness over time if treatment is not continued or if other therapeutic techniques are not used.
2. Other Conditions Treated with CBT
Anxiety Disorders: CBT continuously shows great efficacy in treating a range of anxiety problems. Large effect sizes are shown by meta-analyses for diseases such as social anxiety disorder, panic disorder, and obsessive-compulsive disorder (OCD). Long-term symptom reduction and preservation of treatment benefits are common outcomes of cognitive behavioral therapy (CBT), which frequently outperforms pharmaceutical therapies.
Depression: The efficacy of CBT for depression is mixed. While some studies show strong evidence for its effectiveness, others suggest weaker support, possibly due to publication bias or variability in study quality. CBT has proven to be effective in treating depressive symptoms, but its superiority over other treatments, particularly pharmacological options, is still debated. Long-term outcomes for depression with CBT are generally positive but require more extensive research.
Obsessive-Compulsive Disorder (OCD): When paired with response prevention and exposure strategies, CBT has been shown to have significant benefits in treating OCD. When compared to other treatments like medication alone, this combo approach typically yields better results. Positive results frequently result in significant gains in day-to-day functioning and symptom alleviation.
Eating Disorders: CBT has been shown to be noticeably more successful for bulimia nervosa (an eating disorder where binge eating is compensated by restrictive behaviors) than other psychotherapies, like hypno-behavioral therapy or interpersonal therapy. Higher rates of remission and improved overall symptom control are the outcomes. Though nevertheless beneficial, CBT's efficacy for other eating disorders—like binge eating disorder—is less noticeable than those of other therapies.
Substance Abuse and Addiction: CBT is useful in the treatment of several substance use disorders, especially those involving nicotine and cannabis dependency. As with other interventions, such as medication or contingency management, its efficacy is, however, very low, particularly when it comes to drugs like alcohol and opioids. Promising results have been observed when using CBT to help smokers quit; it frequently outperforms nicotine replacement therapy.
In conclusion, CBT is a strong and adaptable therapy strategy that has shown promise for treating a variety of mental health issues. It works wonders for treating OCD, eating disorders, and anxiety disorders, but it is not as good for treating depression and substance misuse. Its use as a first-line treatment for many illnesses is supported by the data; however, further research and improvement are required to improve its effectiveness and applicability.
Challenges and Limitations of CBT
The paper Perception and Barriers to the Use of Cognitive-Behavioral Therapy in the Treatment of Depression in Primary Healthcare Centers and Family Medicine Clinics in Saudi Arabia explores the resistance and challenges of Cognitive Behavioral Therapy (CBT) due to certain cultural factors. For instance, patient resistance can take many different forms, which can affect how well CBT is adhered to and how effective it is. These are some of the factors that affect patient resistance:
Lack of Training and Knowledge: Although doctors have a favorable opinion of CBT, a major obstacle is that they are not well-trained or educated in it. The effectiveness of CBT implementation is hampered by the fact that many family medicine physicians (FMPs) and general practitioners (GPs) have not received sufficient training in the technique. Patients who may be dubious about CBT may interpret this lack of training as resistance because it could result in a lack of confidence in applying the therapy.
Time Constraints: Research indicates that 59.5% of individuals receiving this treatment felt that cognitive behavioral therapy required too much time. Patients may experience delays or not have enough time for their therapy sessions as a result of this perspective, which could cause resistance or lower therapeutic engagement.
Limited Awareness and Understanding: There are hints that some doctors are not entirely persuaded of CBT's efficacy or validity—roughly 33% doubt the legitimacy of its evidence foundation. Patients' opinions may be affected by this cynicism, which may lessen their desire to participate in CBT.
Furthermore, cultural and socioeconomic factors play a significant role in the accessibility and implementation of CBT. These include:
Training and Education: The study shows that different doctors receive different types of CBT training, with younger doctors being more likely to have received it. This disparity may be a reflection of more general cultural and systemic problems with healthcare professional education, which could impact the accessibility of CBT across diverse geographic areas or demographic groups.
Healthcare Accessibility: The study focuses on the problems with accessibility in the Saudi medical system. The prevalence of depressive symptoms among patients (49.9%) is significantly higher than the percentage of primary healthcare centers that assess and treat mental health issues (20%), indicating a clear mismatch between patient requirements and accessible resources. The lack of qualified cognitive behavioral therapy (CBT) practitioners exacerbates this accessibility problem and limits the availability of effective treatment for various population groups.
Cultural Perceptions: Cultural perspectives on psychotherapy and mental health may also be a factor in the difficulties encountered when applying CBT. Cultural stigmas or misconceptions regarding mental health therapies may affect a patient's willingness to interact with CBT.
Lastly, technological barriers can hinder the implementation and accessibility of CBT. These barriers include:
Digital Divide: Despite the availability of scalable and affordable online cognitive behavioral therapy tools such as MoodGym, the digital gap remains a problem (approximately a third of the world population remains without access to the internet in 2024). The ability of patients and clinicians to access and use technology successfully is a prerequisite for access to such digital resources. For many patients and healthcare professionals, there may be substantial obstacles due to limited internet access or low digital literacy.
Integration into Practice: Online cognitive behavioral therapy (CBT) programs are a useful tool, but integrating them into regular primary care practices calls for further work. Patients require assistance in gaining access to and making use of these resources, and providers require training on how to successfully integrate these digital tools into their practices. The results of the study on providers' time constraints and lack of training may make it more difficult to use digital CBT tools effectively.
Although cognitive behavioral therapy (CBT) is acknowledged as a successful treatment for mental health problems, its application in primary healthcare settings is hampered by a number of issues and constraints. By removing these obstacles, CBT can become more widely used and effective. Some ways to do this include improving training, integrating technology better, and providing more access to mental health resources.
Conclusion
In conclusion, Cognitive Behavioral Therapy (CBT) has solidified its position as a critical treatment strategy for a range of mental health issues. Since its inception, CBT has experienced substantial development, embraced technological breakthroughs to improve its efficacy, and augmented its accessibility. Its fundamental rationale, which centers on changing unhelpful thought patterns and actions, has proven extensively helpful in the treatment of psychological disorders. The versatility of CBT is demonstrated by the various platforms on which it is used, including digital tools that increase its accessibility and practicality.
Digital CBT platforms have increased accessibility and offered helpful support, but they also emphasize the indispensable role of human therapists in addressing the intricacies of emotional reactions and customizing interventions to meet the needs of each patient. Future plans for mental health care delivery appear bright when technology and conventional CBT techniques are combined. This allows for a more thorough and individualized approach. Even with its achievements, further research is critical in improving CBT techniques and making it a viable, impactful, and result-oriented psychotherapy treatment for the affected people to deal with current issues, and make sure the treatment is still applicable and useful.
Authors
References
Aguilera, Adrian, and Frederick Muench. “There’s an App for That: Information Technology Applications for Cognitive Behavioral Practitioners.” The Behavior Therapist / AABT, vol. 35, no. 4, 1 Apr. 2012, pp. 65–73, www.ncbi.nlm.nih.gov/pmc/articles/PMC4270287/.
AlHadi, AhmadN, et al. “Perception and Barriers to the Use of Cognitive-Behavioral Therapy in the Treatment of Depression in Primary Healthcare Centers and Family Medicine Clinics in Saudi Arabia.” Journal of Family and Community Medicine, vol. 28, no. 2, 2021, p. 77, https://doi.org/10.4103/jfcm.jfcm_494_20.
Chand, Suma P, et al. “Cognitive Behavior Therapy (CBT).” National Library of Medicine, StatPearls Publishing, 2023, www.ncbi.nlm.nih.gov/books/NBK470241/.
Fenn, Kristina, and Majella Byrne. “The Key Principles of Cognitive Behavioural Therapy.” InnovAiT: Education and Inspiration for General Practice, vol. 6, no. 9, 6 Sept. 2013, pp. 579–585, journals.sagepub.com/doi/full/10.1177/1755738012471029, https://doi.org/10.1177/1755738012471029.
Hofmann, Stefan G., et al. “The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-Analyses.” Cognitive Therapy and Research, vol. 36, no. 5, 2012, pp. 427–440, www.ncbi.nlm.nih.gov/pmc/articles/PMC3584580/, https://doi.org/10.1007/s10608-012-9476-1.
Pietrangelo, Ann. “9 CBT Techniques for Better Mental Health.” Healthline, 12 Dec. 2019, www.healthline.com/health/cbt-techniques.
Wilhelm, Sabine, et al. “Cognitive-Behavioral Therapy in the Digital Age: Presidential Address.” Behavior Therapy, vol. 51, no. 1, Jan. 2020, pp. 1–14, https://doi.org/10.1016/j.beth.2019.08.001.
Wolters, Lidewij H., et al. “How Can Technology Enhance Cognitive Behavioral Therapy: The Case of Pediatric Obsessive Compulsive Disorder.” BMC Psychiatry, vol. 17, no. 1, 23 June 2017, bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1377-0, https://doi.org/10.1186/s12888-017-1377-0.